Excision Fistula in Ano
Anal Fistula
An anal fistula usually develops as a result of an anal abscess which is drained or bursts. Around half of people who develop an anal abscess will go onto develop an anal fistula. An anal fistula is a track which forms between the inside of the anus and the skin on the outside. This track will continue to drain pus like material and occasionally faecal matter.
Once a fistula has formed it is very unlikely to heal without treatment. Anal fistulae may also develop as a result of other conditions such as Crohn’s disease.
Symptoms of Anal Fistula
People suffering with an anal fistula will experience the following symptoms
- An opening may be seen or felt near to the anus
- Persisting discharge of pus and sometimes a little blood too
- Anal discomfort
- Skin irritation
How is Anal Fistula Investigated?
The Surgeon will take a full history and carry out a clinical examination. Usually this will involve a rigid sigmoidoscopy and/or a proctoscopy. Often if the doctor is able find the inner and outer openings of the fistula and no special investigations will be required.
If it is not possible to find the fistula or if the problem is longstanding or recurrent, an MRI scan or endoanal ultrasound scan will be recommended.
Sometimes the area may be too uncomfortable to examine then the consultant may recommend carrying out an examination under anaesthetic to confirm the diagnosis, and if possible, the fistula can start to be treated at the same time.
If you are over the age of 40 and have had any bleeding or change in bowel habit the consultant may recommend endoscopic examination of the bowel either by flexible sigmoidoscopy or colonoscopy to ensure that it is otherwise healthy, alongside treating the fistula.
Anal Fistula Treatment
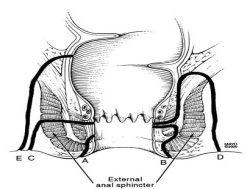
An anal fistula usually requires surgical treatment in order to heal. An anal fistula may often pass through the muscles surrounding the anus. These muscles are important for maintaining continence. It is very important that when fistulae are treated this muscle is not damaged excessively so that a patient has trouble controlling their bowels.
Fistula surgery can be difficult, and some patients may require repeated procedures in order to get their fistula healed. Recurrence is a worldwide problem in fistula surgery and no perfect operation exist. Therefore, there are more than 11 described procedures for fistula surgery. Some patients may need more than one procedure and even in the best hospitals in the world the best success rates for permanent healing on average is only 70%.
Fistula surgery requires a general anaesthetic.
Surgical options that are implemented in Dr Rademan’s practice are:
1.Seton Drainage: Simple drainage involves the insertion of a soft drainage tube known as a seton through the fistula track. The seton suture connects the internal and external openings and the idea is to cause drainage of all the “pockets” of pus next to the tract and also to cause the tract to “mature” so that a sphincter saving procedure can be planned for on average x3 months after the placement of a draining seton suture. This seton can also stay in place long term and some patients are happy to have a seton in place indefinitely.
2.Laying open the fistula (fistulectomy): This involves cutting out/open the fistula track. It is useful for those fistulae that don't pass through the sphincter muscle or only a small part of it (usually < 1cm of muscle involved).
3.Muscle Sparing treatments (sphincter saving):
- Successful treatment of a fistula-in-ano should be aimed at closing the internal opening (the origin of the fistula) and treating the fistula tract without causing anal incontinence.
A). Options to close the internal opening:
i). A rectal mucosal flap or a rectal full thickness flap to close the opening after debridement and simple suturing of the internal opening. The rectal flaps do have a small risk of causing anal incontinence, especially if the surgery/opening is too close to the anal sphincters (+/-13%).
ii). OTC clip – it is a metallic (titanium) clip that is placed over the internal opening by a device and may be removed at 3 months or left in place if successful.
B). Options to remove/close the fistula tract:
i). Laser Treatment (With FiLaC®): To treat anal fistulas as muscle-sparing as possible, now there is FiLaC® laser therapy of the fistula tract.
During laser therapy, defined energy will be led into the fistula tract with help of an innovative laser probe. By this, the fistula tissue will be destroyed in a most sparing way and has not to be tediously extracted during a complex surgery by a surgeon.
The laser probe is slowly pulled back step by step like a zipper, and the fistula is being closed. The highly flexible probe is suitable for the application even in wound tracts and can be applied independently from the length of the fistula tract.
The laser treatment takes only a few minutes and provides the possibility to completely spare the enucleation of the fistula out of the healthy tissue.
ii). LIFT procedure: Enucleation of the fistula tract and tying off the tract as close to the internal opening (intersphincteric) as possible.
iii). VAAFT procedure: it is an endoscopic procedure that entails direct vision of the fistula tracts and pockets of pus and cauterization and debridement under direct vision of both. A draining seton is not required before surgery.
